Code Alerts: Color vs Plain Language
Confident your Hospital is Prepared to Respond to an Emergency Code?
April 2023
By Jody Randall MSN, RN, CIC, HACP-CMS, HACP-PE
CEO and Founder
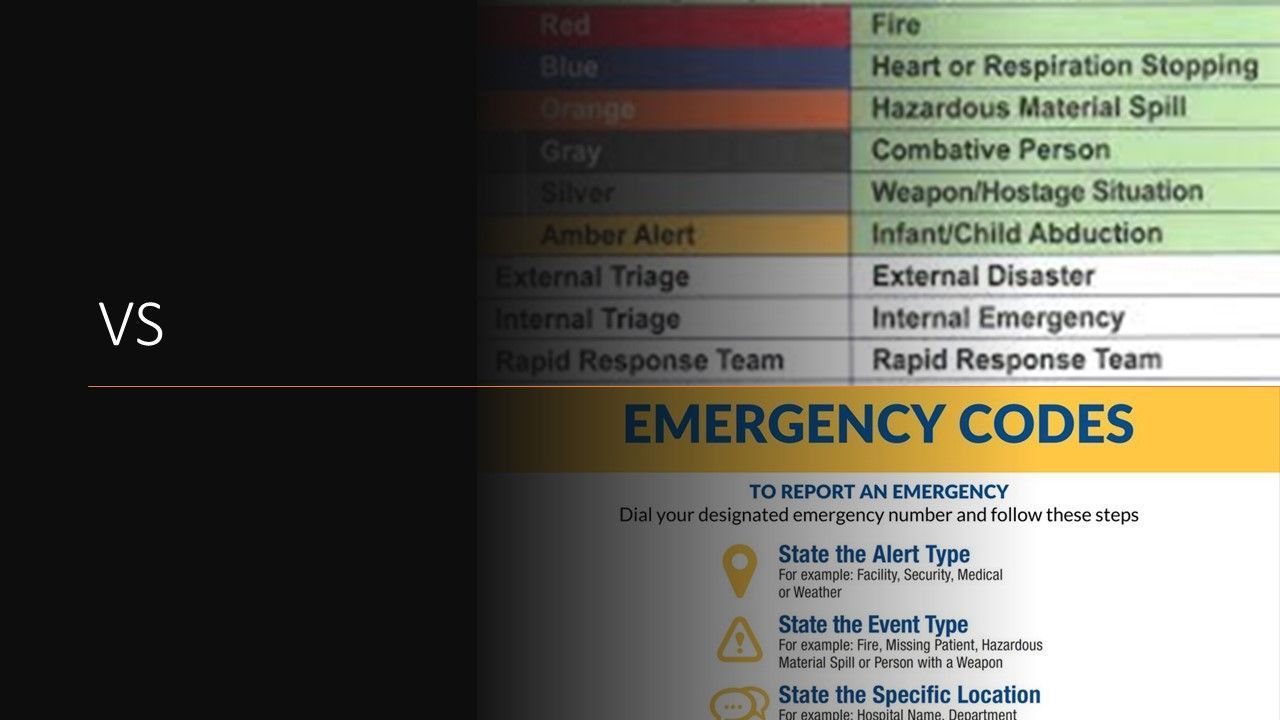
You do not necessarily have to work in the healthcare industry to know that if a “code blue” is called, it is to alert healthcare providers that a patient has gone into cardiac arrest. Color codes have been around for decades in healthcare. It is a system used to announce various types of situations that require rapid response, emergency treatment, surveillance and security. Depending on the type of emergency, response to this type of announce may impact a single location or can be a facility-wide catastrophic event.
There has been a deviation from the use of color codes by many healthcare organizations. Plain language codes have not only been adopted by hospitals, but are supported by the US Department of Homeland Security and the American Hospital Association. The U.S. Department of Health & Human Services also supports the plain language movement and has published a white paper on its website that includes this statement:
“There are currently no governmental or regulatory requirements, that the authors are aware of, that mandates the use of plain language in daily operations of individual organizations such as healthcare facilities. However, with new CMS emergency preparedness regulations regarding a healthcare facility’s communication plans complying with all federal and state laws and the facility’s ability to effectively communicate “within the facility, across health care providers, and with State and local public health departments and emergency systems” (Centers for Medicare & Medicaid Services, 2016) it could be argued that a standardization of emergency codes within healthcare facilities is now a mandated step in the emergency communication process.”(Prickett, K.J. and Bellino, J., 2019)
Our HCE professionals have found that although many organizations have adopted the plain language emergency code system, that may not be the majority. It is not uncommon to find that hospitals are still following the color emergency code system. One alleged disadvantage of continuing use color codes include lack of knowledge by personnel of what each of the colors mean.
There has been a great deal of argument that with the increasing number of traveling staff, there is not an opportunity to effectively train interim personnel on the meaning of each of the color codes. When color codes are the emergency code system being used, you will likely find that personnel have a badge buddy reminder to assist them with the definitions of each of the color codes. Ultimately, regardless of the emergency response protocol used, it is only as good as the training that goes along with it.
Our HCE experts found this lack of conformity by all to plain language worth further investigation. In talking with emergency response personnel and law enforcement officials, we learned that they are in support of plain language emergency codes. They emphasized that all people should have an equal opportunity to save themselves. In the tragic event that an active shooter enters a facility, patients and visitors would not necessarily know the meaning of a “code silver”. Although we questioned officials about plain language leading to panic ensuing, we felt that their counterarguments were strong and valid. One emergency response professional responded by saying that healthcare professionals are trained and work hard to save lives, it is not ethical or expected for them to risk life or limb to do so in this situation. Another emergency response trainer also suggested that when calling plain language codes such as bomb threat, active shooter, or a hostage situation that once the plain language code is called, their heightened alertness response by all would actually help to disintegrate the threat faster.
Whether or your organization uses plain language codes or color codes to alert of emergency situations, it is clear that proper training of personnel and performing drills periodically are the best way to prepare your organization for any unplanned emergent event. We understand that healthcare organizations today are facing tremendous pressures just to ensure adequate resources are available for day-to-day operations. But unfortunately, these are the times we are in and being prepared to face these alerts is the duty of the facility and their leadership.
We also know that training and conducting emergency drills have taken a back seat in many facilities while organizational needs are being prioritized. We respectfully request that you make your emergency response plan a high priority before an unplanned event should occur. Our dedicated healthcare heroes out there deserve nothing less.
HCE is Here to Help
Healthcare Consulting Experts LLC was built based upon our understanding of the challenges that healthcare facilities are facing today. Healthcare professionals strive to deliver the best possible care to all patients. We can help your facility through the difficult times and put you back on track to a less stressful tomorrow.
Don’t take chances! Our experts can assist with regulatory compliance requirements for whether you are building a new, state-of-the-art project or renovating an existing structure. Be sure to visit
Our Website
to see a full list of the services that we provide.
Contact us today at +1 (800) 813-7117 for a free initial consultation.
Please join us by clicking on any of our icons below to leave a comment or for more informati
on and updates.
References:
https://www.medicare.gov
https://cdn.ymaws.com/www.iahss.org/resource/resmgr/docs/WhitePaper_Plain_Language_Em.pdf
https://www.jointcommission.org/





