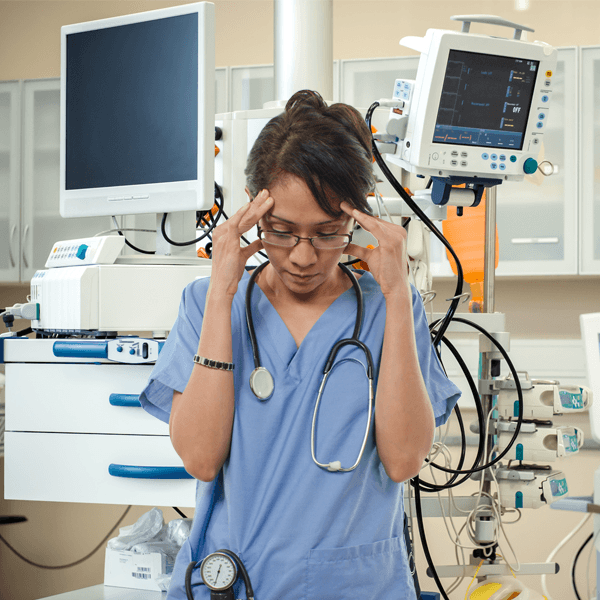
Alarm Fatigue ... Don't Get Caught Being Silent
Considerations For Facilities to Successfully Battle Alarm Fatigue
august 2022
By Jody Randall MSN, RN, CIC, HACP-CMS, HACP-PE
CEO and Founder
Alarm fatigue is not a new phenomenon. This occurs in a variety of setting but is more common in critical care settings when clinicians become desensitized by countless alarms, many of which are false or clinically irrelevant. Technological advancements continue to evolve in the health care industry. With numerous monitoring devices to assist with patient care, it is important to consider the risk associated with utilization of monitoring devices.
The development of alarm fatigue is not surprising. In this
cited study (1) , there were nearly 190 audible alarms each day for each patient. Here are a few examples of contributing factors:
- Multiple monitoring devices being used simultaneously
- Incorrect alarm parameters
- Poor connection of monitoring equipment
- Responding to false alarms
- Insufficient staff education on safe monitoring practices
Focus on alarm fatigue may be glazed over in clinical settings today while recent emergent matters have received greater attention. The Joint Commission (TJC) made alarm safety a National Patient Safety goals in 2014 and it continues to be considered a high priority. National Patient Safety Goal 6 -
Reduce Patient Harm Associated With Clinical Alarm Systems
- is still in effect today. The
objective of NPSG.06.01.01 is to improve the safety of clinical alarm systems (2) . Patient harm and even death continue to occur today in patient care settings due to alarm fatigue.
Considerations for Developing Safe Practices
Leadership accountability is becoming even a greater focus in the healthcare industry today. Development of policies and procedures concerning alarm safety is critical. It is important for those in leadership roles to be involved in all matters related to alarm system safety. Another consideration is to obtain input from providers on safe parameters for patients who require monitoring. For example, a patient who is tachycardic or hypertensive may need to have alarm parameters adjusted, as they may never achieve normal range parameters which could essentially lead to constant alarming.
Areas that should be addressed when creating or revising policies and procedures:Range settings for equipment
- Personnel authorized to adjust equipment parameters
- Preventative maintenance check frequency
- Personnel authorized to silence alarms
- Personnel authorized to turn off equipment parameters
- Guidance for safely setting up and using patient care equipment
It is Never Acceptable to Silence Alarms Without Evaluating the Cause of an Alarm.
Education
In order to prevent adverse events from occurring, staff education must also be included in alarm safety programs in all facilities. Developing policies and procedures system may not be enough to engage end-users in alarm system safety best practices. Eliciting feedback from staff on alarm frequency and false alarms is important. If concerns go unheard or are not addressed, staff may disengage due to lack of concern from leadership.
Staff should not only be educated on equipment but also deemed competent on safe use of equipment. As part of taking over a patient assignment at change of shift, a routine check of all monitoring equipment should be done by the nurse taking over care. Bedside reporting can help to provide oncoming nurses with a better understanding of equipment in use. Ideally, patients should be included in the plan of care. This provides a better understanding of why equipment is being used and what the patient is being monitored for. If there is an audible alarm and the patient is not in distress, if there is not a response to the alarm, the patient can be instructed to use a call light to alert nursing personnel.
Patients should always be assessed for worsening conditions of health so that life saving interventions can be initiated immediately. If a patient is not in distress upon assessment, then an evaluation of equipment connections and equipment should be completed. If it is discovered that any form of patient equipment is not working correctly, then equipment should be replaced with equipment that is working properly. Faulty equipment should be tagged-out of service and Bio-Med should be notified immediately.
Not addressing alarm fatigue will be sure to lead to more alarm fatigue nursing burnout and an increased risk of patient harm and death. Technology will continue to have a major role in patient care. Medical equipment and monitoring devices will continue to evolve and emerge. It is critical that healthcare leaders take the time to develop an alarm system safety program. If a program is already in place, then it is important to conduct a risk assessment of your organization to determine how effective the system truly is.
We can help! Let our experts help you to avert risk of burnout and harm. Contact HCE for a free consultation.
References:
- Drew BJ, Harris P, Zegre-Hemsey JK, et al. Insights into the problem of alarm fatigue with physiologic monitor devices: a comprehensive observational study of consecutive intensive care unit patients. PLoS One. 2014;9:e110274.
- www.jointcommission.org/-/media/tjc/documents/standards/national-patient-safety-goals/2022/simple_2022-cah-npsg-goals-101921.pdf
HCE is Here to Help
Healthcare Consulting Experts LLC was built based upon our understanding of the challenges that all healthcare facilities are facing today. Healthcare professionals strive to deliver the best possible care to all patients. We can help your facility through the difficult times and put you back on track to a less stressful tomorrow.
Don’t take chances! Our experts can assist with regulatory compliance requirements for whether you are building a new, state of the art project or renovating an existing structure. Be sure to visit
Our Website
to see a full list of the services that we provide. Contact us today at +1 (800) 813-7117 for a free initial consultation.
Please join us by clicking on any of the icons below to leave a comment or for more informati
on and updates:





